Michelle Henderson & Brigitte Collins
The Decision Guide is now widely used by healthcare professionals (HCPs) in clinical practice to guide decision making when starting rectal irrigation. However, if we go back a step – how do you know whether or not your patient is ready to start rectal irrigation in the first place? If we start the right patients on rectal irrigation, at the right time, then the outcomes would surely be even more positive?
This is something the clinical team have been thinking about a lot recently, researching and discussing this concept of psychological readiness.
So what is it…
Psychological readiness is about being in the right frame of mind to undertake a new activity, in this case, learning and using rectal irrigation. It takes into account both mental and emotional factors of the individual, involving a combination of mental strength, emotional stability, confidence and adaptability. Achieving psychological readiness might involve learning a new task (e.g rectal irrigation) and also the development of coping strategies to handle any challenges that may arise.
Can psychological readiness be applied in the healthcare setting?
Yes it can and it’s important for both patients and HCPs.
For the patient, where the next step in their treatment pathway is rectal irrigation, by assessing their psychological readiness, we can prepare them both mentally and emotionally so that they are ready to learn how to use rectal irrigation. This could lead to improved adherence, better results, a more positive irrigation experience, with the potential for enhanced quality of life long term.
Clinicians also face challenges and need to be psychologically ready to teach irrigation and support the patient. Having access to training, support and resources such as product literature, step-by-step guides and the Decision Guide enable HCPs to deliver high quality effective care.
Promoting psychological readiness in healthcare involves:
- Open and honest communication between the HCP and the patient so that patients feel comfortable asking questions and expressing their concerns.
- Patient education – about their condition, treatment plan and what to expect. This helps alleviate anxiety and uncertainty.
- Offering emotional support to patients, acknowledging their feelings and fears through active listening and reassurance.
- Informed consent -so that patients have a clear understanding of the risks, benefits and alternatives associated with their treatment.
- Psychosocial assessment – to identify those patients who may be at risk of significant psychological distress. This allows for targeted interventions and support. In the context of rectal irrigation, this is particularly important for patients who have suffered abuse.
- Planned follow-up – the importance of this should not be underestimated, patients should leave their consultation with a clear plan and know how to access ongoing support and resources.
So overall, achieving psychological readiness in a healthcare setting requires a patient centred approach to build a compassionate and supportive care environment, with a focus on both the psychological and emotional needs of the individual and also the HCP.
How do we measure psychological readiness?
This is not a new concept, having been used for a long time in the field of sports psychology. It is measured through a set of questions, statements or skills. It’s a simple and intuitive way to capture subjective perceptions and readiness levels.
Can we use these scales to measure psychological readiness in relation to bowel function?
Yes we can.
Brigitte says “When I worked at Saint Marks, I didn’t think about psychological readiness – I would happily send a patient off with rectal irrigation regardless of whether they were ready to use it or not. Unsurprisingly, sometimes the product would sit unused in the patient’s home, leading to frustration on both sides – and unnecessary cost to the NHS”
We hosted a panel discussion at the Bladder and Bowel Symposium 2023 in Coventry around psychological readiness. All of our panellists agreed how useful it could be in this field.
“…using numbers (on the scale) gives a quick synopsis of where the patient is at… gives objectivity…can measure progress …although it’s not really about the numbers it’s a trigger to have the conversation”
Monica, Advance Nurse Practitioner
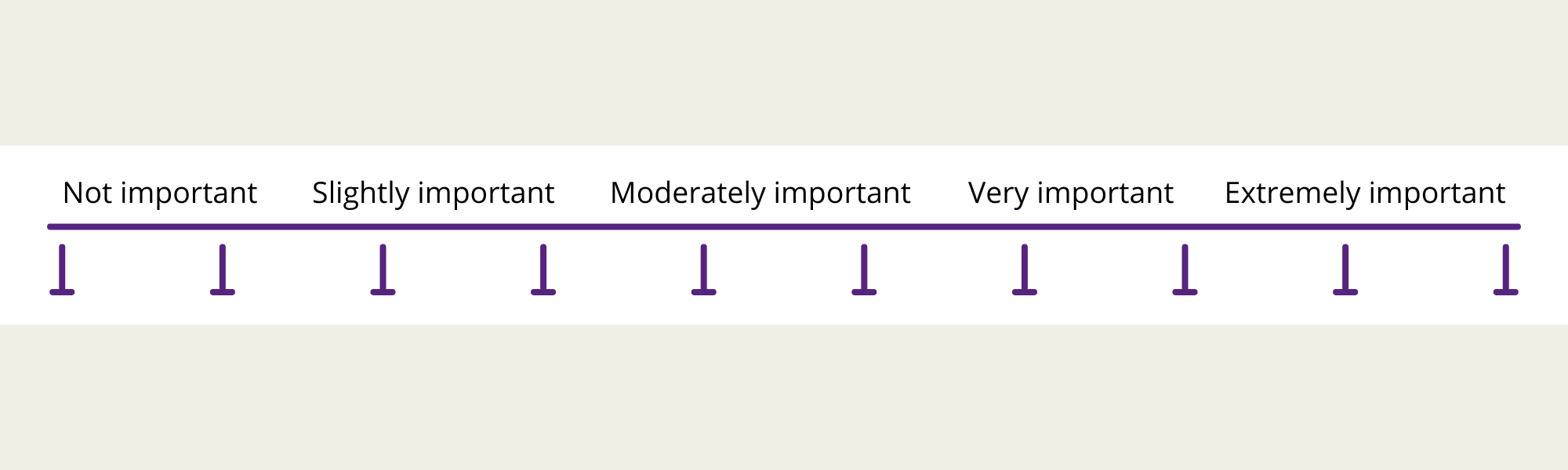
As a result of this discussion, our original ideas for visual analogue scales have evolved into the scales below:
Q1. How important is it to treat your bowel problem?
Q2. How ready are you to use RI as your next treatment option?
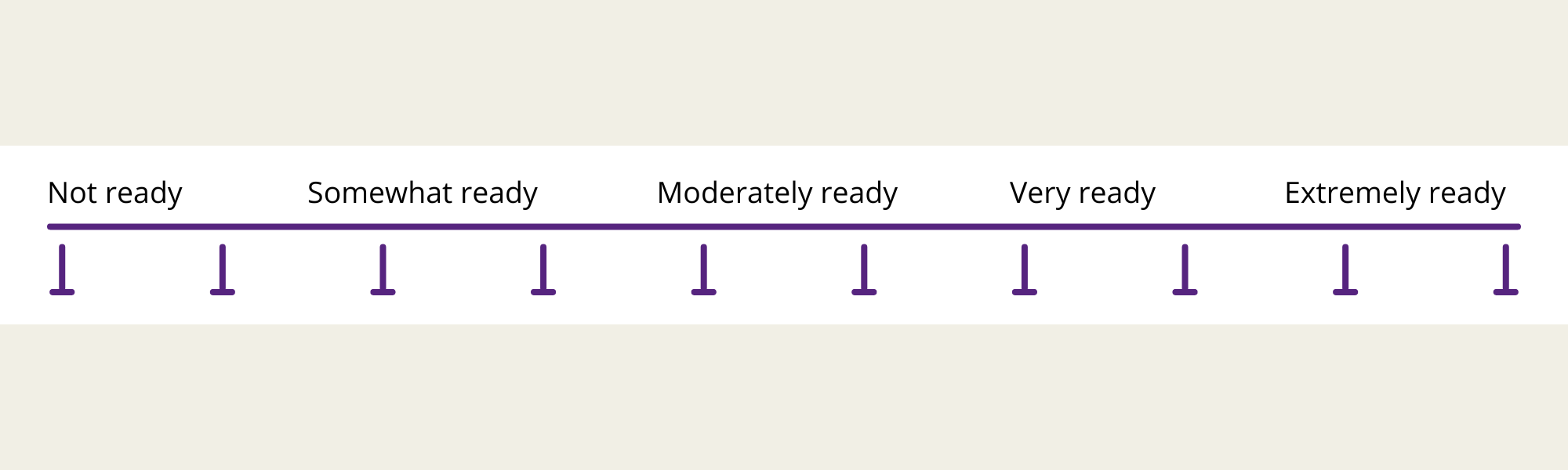
Using these two simple scales can open up the conversation around rectal irrigation. Barriers and anxieties can be identified and talked through, answering patients’ questions and offering reassurance. In this way, the patient is psychologically prepared to learn about and use irrigation. Conversely, the scales might identify that the patient is not ready to start irrigation at this time, giving both the patient and the HCP permission to pause this treatment for now.
“…using words like how do you actually feel about this (rectal irrigation), allows the patient time to bring up their anxieties. It (the scale) opens up the conversation – so you can listen & understand their barriers (to rectal irrigation)”
Jess, Specialist Pelvic Health Physiotherapist
In summary, these psychological readiness scales offer a chance to explore patient’s views:
- Enabling conversation about anxieties/ barriers/ readiness
- Giving permission not to use irrigation
- Improving adherence
- Preventing waste – of time, resources and equipment
What next?
These scales will now be used and evaluated in clinical practice. We will keep you updated with developments.